Peripheral Artery Disease (PAD)
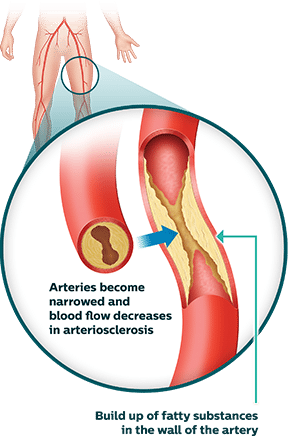
Peripheral artery disease (PAD) is a common condition in which fatty plaque builds up in the arteries. The plaque can harden and reduce the flow of blood to the head, organs, or limbs. Although PAD can occur in any blood vessel in the body, it typically affects the legs, ankles and feet. When blood flow is reduced, patients with PAD may experience uncomfortable symptoms such as leg pain while walking (claudication), reduced pulse, skin temperature changes and pain at rest.1 Over time, the progressive disease can reduce quality of life and mobility. Critical limb ischemia (CLI) is the advanced stage of PAD that may lead to non-healing wounds below the ankle, gangrene and ultimately limb amputation, as well as other serious health complications.2 Patients with PAD are also at risk for the development of stroke and heart attack.3 Learn more about the signs and symptoms of PAD.
Symptoms of PAD
Certain risk factors are associated with PAD, such as smoking, older age, and having certain diseases and conditions, such as diabetes, high blood pressure, history of stroke and coronary heart disease.4 While some patients with PAD experience mild to no symptoms, others may experience exercise pain (claudication), pulse changes, skin temperature changes, pain at rest and non-healing wounds. PAD symptoms include:5

Claudication
Pain, aching, or heaviness in the leg muscles when walking or climbing stairs.

Pulse Change
A reduced or absent pulse in the ankle or foot.

Temperature Changes
A lower skin temperature in one limb compared to the other. The skin may feel cool to the touch.

Pain at Rest
Experiencing pain without physical activity, such as during the night.

Non-Healing Wounds
Sores or wounds on the toes, feet, or legs that aren’t healing well.
Non-healing wound image courtesy of Dr. Raghu Kolluri.
PAD Diagnosis and Treatment
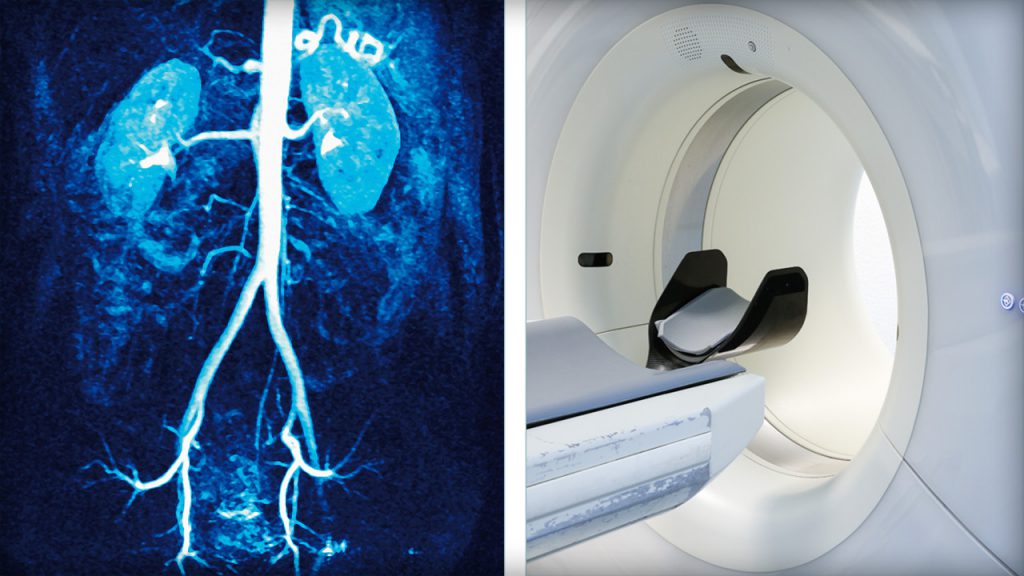
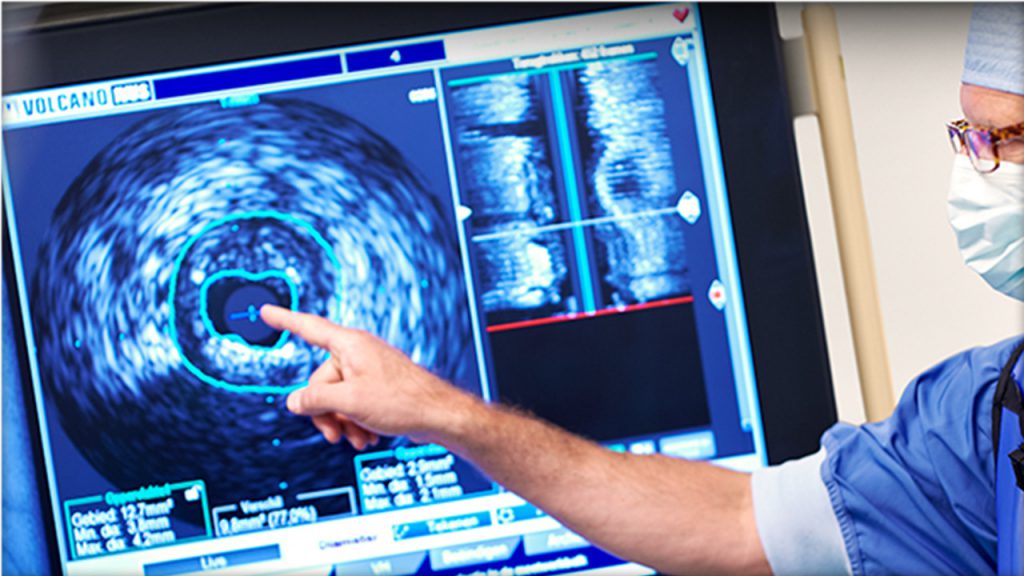
Diagnostic Procedures If you suspect you may have PAD, a proper diagnosis is critical. In addition to a physical exam, blood tests, and patient history, a doctor may use one, or a combination of tests such as: ankle-brachial index at rest and with exercise, duplex ultrasound, CTA angiography, transcutaneous pulse oximetry, MRA angiography and Intravascular Ultrasound(IVUS):6 Photos of Diagnostic Procedures
Videos of Diagnostic Procedures
Intravascular Ultrasound (IVUS)
A special imaging device that uses a small catheter to image the interior of blood vessels and to measure plaque build-up from within the arteries.
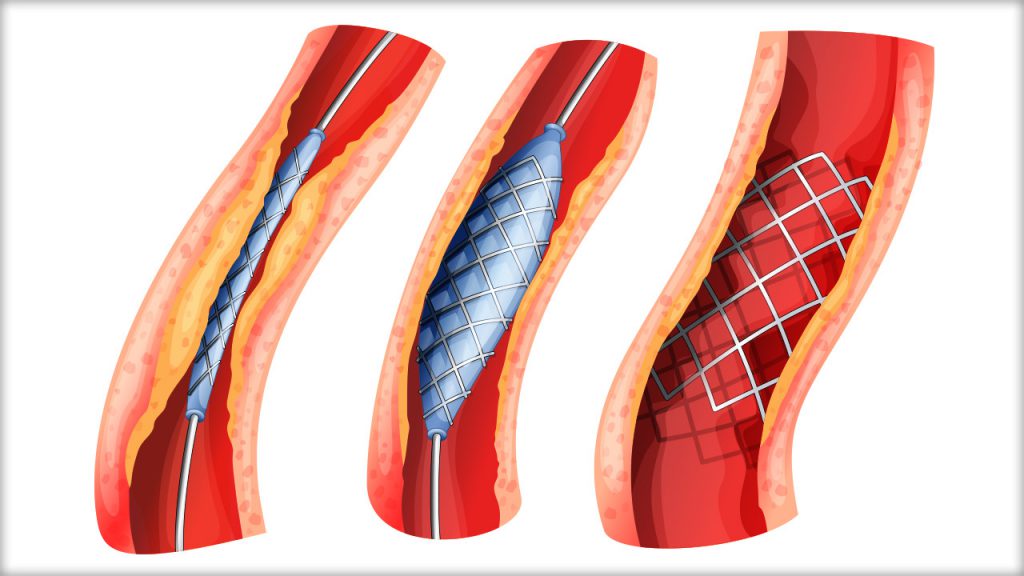
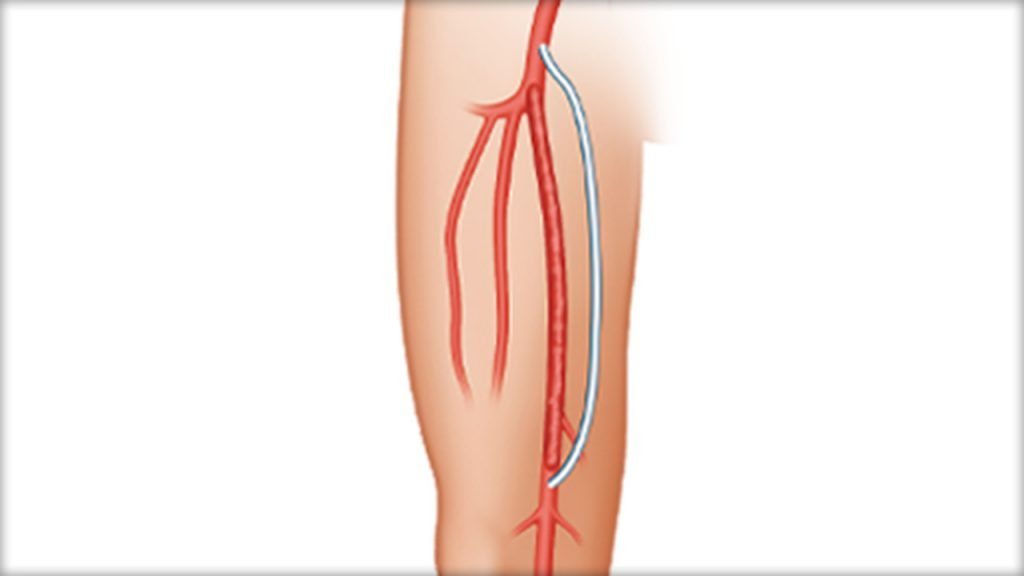
PAD Treatments
Although serious, PAD is treatable. Treatment may focus on reducing PAD symptoms and the progression of plaque build-up. This may be achieved through lifestyle changes, such as exercise, diet and by quitting smoking. If lifestyle changes are not enough, a doctor may recommend one or more of the following treatment options:7 Photos of PAD Treatments
Videos of Diagnostic Treatments
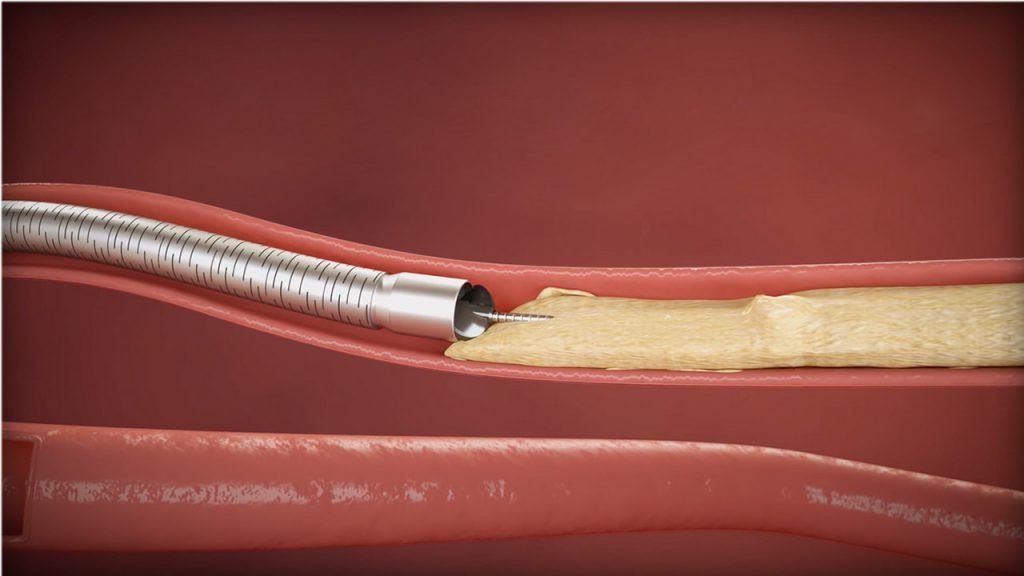
Atherectomy
A procedure that uses a special catheter to remove plaque build-up from a blood vessel. The result is increased blood flow to the peripheral tissue.
Patient Stories: PVD and Me
Peripheral vascular disease can greatly impact a person’s quality of life. Take the next step and learn what it’s like to have PVD from patients and why it’s important to get help. PAD Stories
More Patient Stories
DVT Stories

Deep vein thrombosis (DVT) can strike quickly with little notice. Learn more about Reid’s condition and his road to recovery.
DVD Stories

Patients with deep venous disease (DVD) often go through years of suffering with worsening symptoms and other underlying conditions. Learn about Melanie’s path to uncovering an underlying condition and her road to restoring her health.
CLI Stories

Early intervention can be key for critical limb ischemia (CLI). Learn about Mark’s struggles and triumph to overcome CLI.
Helpful Resources

PVD Doctor
Discussion Guide
Get helpful tips and advice on how to talk to your doctor about a PVD screening.

PAD Brochure
Find out more information on PAD by downloading this helpful brochure.
Third-Party Resources
Helpful Websites
Blogs
Find a Doctor that Treats PAD
If you think you may have PAD, it is important to get help. Talk to your doctor, or use our Doctor Finder tool below to find a PAD specialist near you.
This tool is not inclusive of all specialists. Consult with your insurance provider to find specialists that are covered within your network.
Are You a Healthcare Professional?
Find out how to register your practice with us.
1. “What is Peripheral Arterial Disease?” National Institutes of Health. U.S. Department of Health and Human Services, June 22, 2016 2. Aquarius et al. “Poor health-related quality of life in patients with peripheral arterial disease: Type D personality and severity of peripheral arterial disease as independent predictors.” Journal of Vascular Surgery (September 2007Volume 46, Issue 3, Pages 507–512). 3. “Know the risk factors, signs, treatments, and ways to prevent P.A.D.” NIH Medline Plus. National Institutes of Health and Friends of the National Library of Medicine. Summer 2008 Issue: Volume 3 Number 3 Page 19 4. “Who Is at Risk for Peripheral Artery Disease?” National Institutes of Health. U.S. Department of Health and Human Services, June 22, 2016 5. “What Are the Signs and Symptoms of Peripheral Artery Disease?” National Institutes of Health. U.S. Department of Health and Human Services, June 22, 2016 6. “How Is Peripheral Artery Disease Diagnosed?” National Institutes of Health. U.S. Department of Health and Human Services, June 22, 2016 7. “How Is Peripheral Artery Disease Treated?” National Institutes of Health. U.S. Department of Health and Human Services, June 22, 2016
Disclaimer
The opinions and clinical experiences presented herein are for informational purposes only. Individual results may vary depending on a variety of patient-specific attributes and related factors. Dr. Raghu Kolluri has been compensated by Philips for his services in preparing and providing this material for Philips further use and distribution. We offer links to third-party websites that may be of interest to our website visitors and in no way, represent any affiliation or endorsement of the information provided on those linked websites. These links are provided solely for your convenience and to assist you in learning more information on this topic. However, Philips does not control, endorse or guarantee the accuracy of the information contained on the linked sites. In addition, Philips makes no representations or warranties of any kind with regards to any third-party websites or information contained therein. If you have any questions or concerns about the information on the linked third-party websites, please contact the third-party websites directly.