Superficial Venous Insufficiency (SVI)
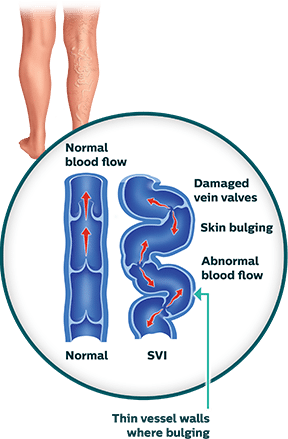
Superficial venous insufficiency (SVI) is a common condition that occurs when there is decreased blood flow from the leg veins up to the heart.1 Without adequate flow, the blood can pool in the leg veins and result in common conditions, such as spider veins, reticular veins and varicose veins. Approximately 25 million people in the United States suffer from varicose veins—enlarged blue, red, or flesh-colored veins that are raised above the surface of the skin.2 Like varicose veins, spider veins are also swollen veins that appear through the skin, but are closer to its surface and resemble tree branches with short, jagged lines. Although spider veins are not usually symptomatic, the accompanying reticular veins, found deeper in the skin, often cause discomfort. Reticular veins are also referred to as “feeder” veins. These vessels are smaller branches which can originate from bigger varicose veins. All three types of venous problems appear on the thighs, backs of the calves, or ankles. Although not life-threatening, SVI can cause problematic skin changes and can progress over time.
Symptoms of SVI
Superficial veins have less muscle support than deep veins, so any condition that puts pressure on the legs or surrounding areas can lead to pooling of blood in the extremities. Common pressure inducers are obesity, pregnancy, and standing for long periods, as well as sitting and limited movement. The likelihood of acquiring SVI increases if other family members have it and with age. Over time superficial veins weaken and aren’t able to push blood back up the heart.3 While some people have minor symptoms that are simply cosmetic, others have more debilitating ones. Common symptoms of SVI are a feeling of heaviness in the legs, aching, swelling, throbbing and itchy skin. Over time this can lead to inflammation of the varicose veins, scaling of the skin and eczema, thickening of the skin and can ultimately result in leg ulcers. SVI symptoms include:4

Tired Heavy Legs
A general heaviness in the legs may indicate that blood is not circulating properly. If left untreated it can lead to progression of the disease.

Pain
A dull diffuse ache or throbbing can occur accompanied by a heaviness that makes it feel as though you are walking in cement shoes.

Swelling
Superficial Venous Insufficiency (SVI) may cause swelling in the affected vein area.

Skin Changes
When blood pools in the legs, the skin of the affected area becomes darkened. Itchy skin or eczema may develop as well as a thickening of the skin.
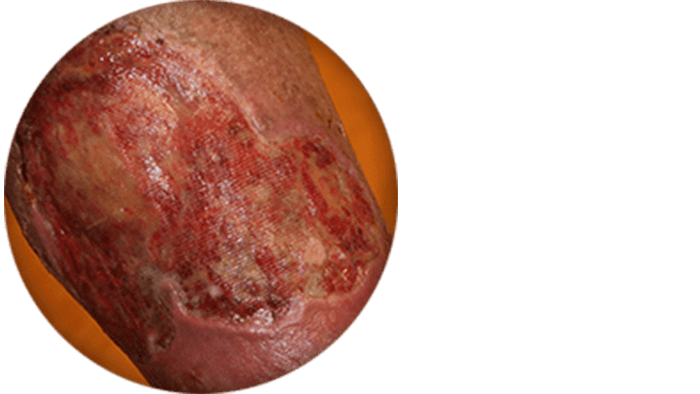
Ulcers
In severe cases, ulcers may develop when pooled blood causes tissue damage.
Swelling, skin changes, and ulcer images courtesy of Dr. Raghu Kolluri.
SVI Diagnosis and Treatment
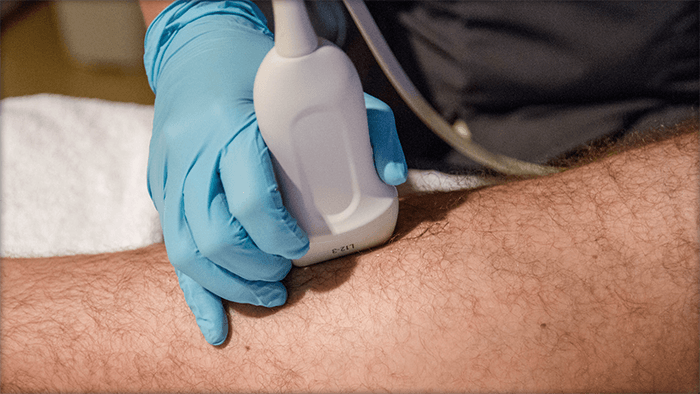
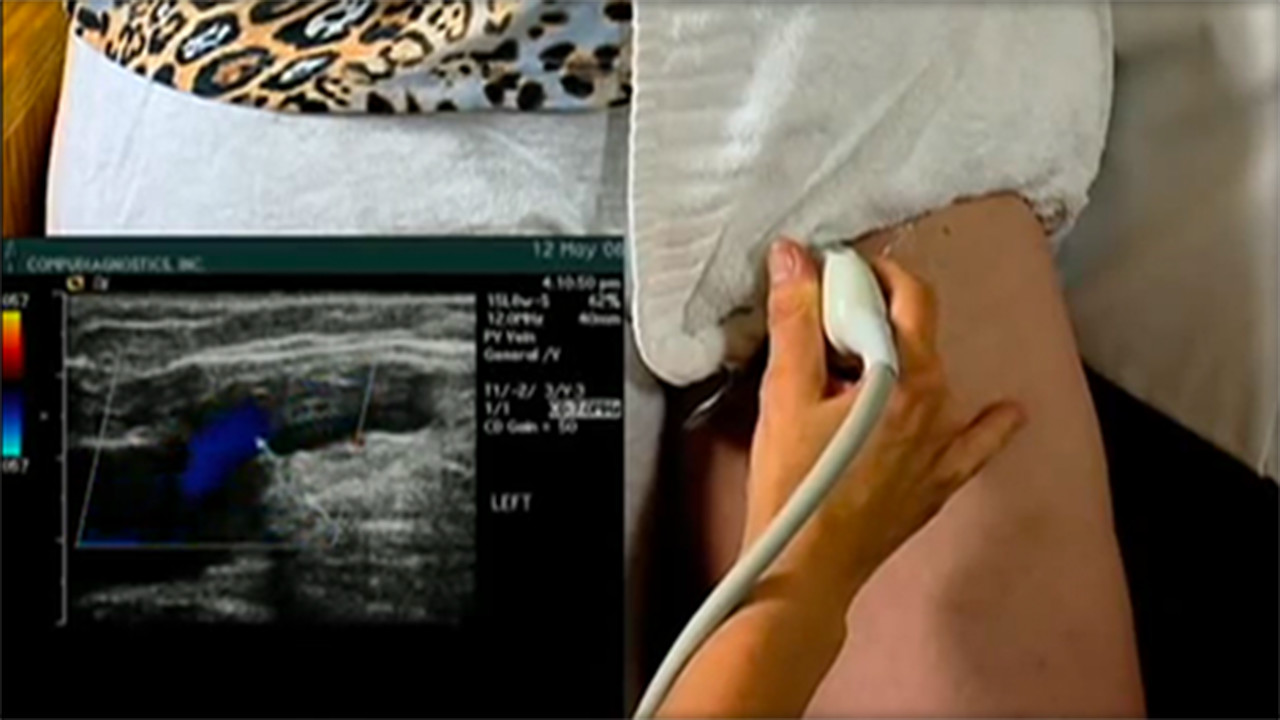
Diagnostic Procedures Superficial venous problems may be visible on the legs, but it is important to let a doctor confirm a diagnosis. Sometimes SVI can be indicative of other problems in the deep veins, such as deep venous obstruction and a doctor will need to determine if it is DVO or SVI. To confirm SVI, and to locate the source of insufficiency, a doctor may use a combination of physical exam, medical history and one or more of the following tools:5 Photos of Diagnostic Procedures
Videos of SVI Diagnostic Procedures
Duplex Ultrasound
This is a non-invasive test which uses sound waves to create a color map of the blood vessels and examines blood flow in your legs.
SVI Treatments
There are multiple ways to manage SVI, depending on the extent of the diseased veins. For some people, changes like adopting a healthy diet and increasing exercise can help reduce the pressure around the legs thereby reducing the progression of varicose veins.
Seeking treatment can be strictly cosmetic while other people will wait until they have pain or ulcers. If you are experiencing symptoms that bother you discuss this with your doctor, because they can potentially lead to leg ulcers.
After consulting your doctor, he may recommend the following treatments:
Photos of Treatments
Videos of SVI Diagnostic Procedures
Sclerotherapy
A common treatment for both spider, reticular and varicose veins where a doctor uses a needle to inject a liquid chemical into the vein. The chemical shuts down the vein and the blood can find an alternate way back to the heart.
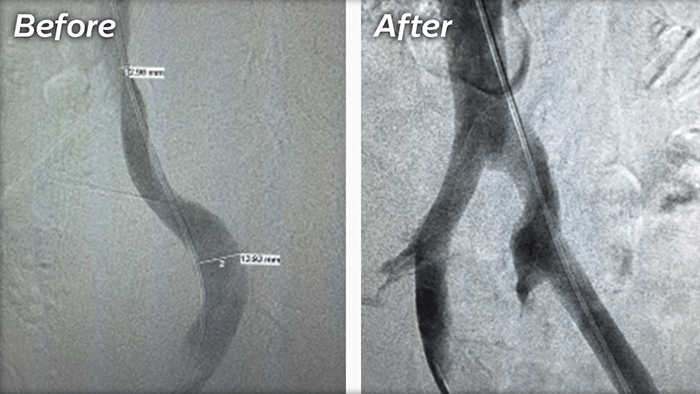
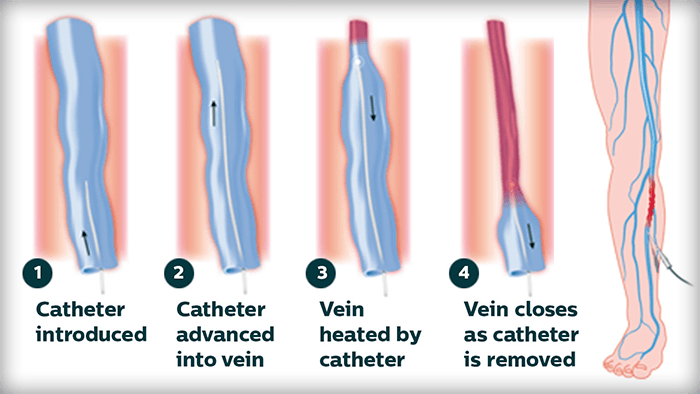
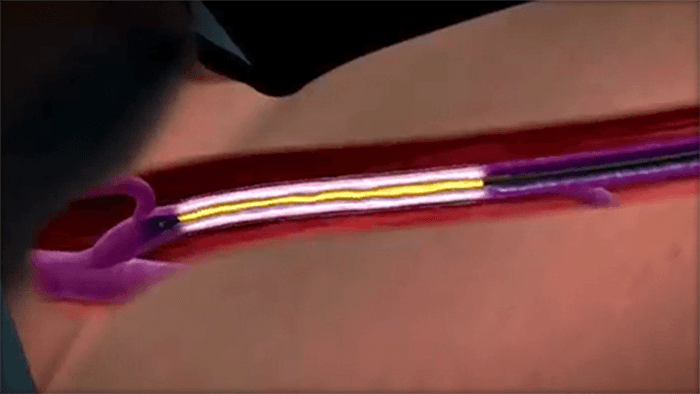
Ablation Therapy
A minimally invasive treatment that uses lasers, radiofrequency, non-thermal ablation or mechanochemical ablation to shut down large varicose veins in the legs.
PVD & Me: Patient Stories
Read the inspiring stories of real patients with various conditions of PVD. Learn about their diagnosis, treatment and journey to regaining their quality of life.
DVT Stories
Deep Vein Thrombosis (DVT) can strike quickly with little notice. Learn more about Reid’s condition and his road to recovery.
CLI Stories
Early intervention can be key for critical limb ischemia (CLI). Learn about Mark’s struggles and triumph to overcome CLI.
PAD Stories

Many PAD patients experience a gradual decline in activity level and quality of life which can go unnoticed for years. Learn about Joe’s suspicions and his perseverance to seek help.
DVD Stories

Patients with Deep Venous Disease (DVD) often go through years of suffering with worsening symptoms and other underlying conditions. Learn about Melanie’s path to uncovering an underlying condition and her road back to restore her health.
Helpful Resources

PVD Doctor
Discussion Guide
Get helpful tips and advice on how to talk to your doctor about a PVD screening.

SVI Brochure
Find out more information on SVI by downloading this helpful brochure.
Third-Party Resources
Helpful Websites
Blogs
Find a Doctor that Treats SVI
Consult your doctor to learn more about SVI and how to maintain your vein health. You can also use our Doctor Finder tool below to find a specialist near you.
This tool is not inclusive of all specialists. Consult with your insurance provider to find specialists that are covered within your network.
Are You a Healthcare Professional?
Find out how to register your practice with us.
1. Weiss et al. “Venous Insufficiency.” Medscape. May 26, 2016 2. Eberhardt et al. “Chronic Venous Insufficiency.” Circulation. 2014;130:333-346. July 21, 2014. 3. “Varicose veins and spider veins.” Office on Women’s Health. U.S. Department of Health and Human Services. January 04, 2017. 4. Lin et al. “The Management of Varicose Veins.” Int Surg. 2015 Jan; 100(1): 185–189. 5. “How Are Varicose Veins Diagnosed?” National Heart, Lung and Blood Institute. U.S. Department of Health & Human Services. Feb. 14, 2014.
Disclaimer
The opinions and clinical experiences presented herein are for informational purposes only. Individual results may vary depending on a variety of patient-specific attributes and related factors. Dr. Raghu Kolluri has been compensated by Philips for his services in preparing and providing this material for Philips further use and distribution. We offer links to third-party websites that may be of interest to our website visitors and in no way, represent any affiliation or endorsement of the information provided on those linked websites. These links are provided solely for your convenience and to assist you in learning more information on this topic. However, Philips does not control, endorse or guarantee the accuracy of the information contained on the linked sites. In addition, Philips makes no representations or warranties of any kind with regards to any third-party websites or information contained therein. If you have any questions or concerns about the information on the linked third-party websites, please contact the third-party websites directly.