Tired, Heavy Legs

Symptom Details
At some point, most people experience tired, heavy legs—after a tough workout, during pregnancy, or after sitting for long periods of time. But when the discomfort becomes chronic and persistent, it may signify an underlying venous or arterial condition such as superficial venous insufficiency (SVI) or deep venous insufficiency (DVI), and to a lesser extent peripheral artery disease (PAD).
Venous 3,4,5
Similar to arterial conditions, venous disease can also produce leg discomfort. Common symptoms of SVI are a feeling of heaviness in the legs, aching, swelling, throbbing.3,4 The pain may be exacerbated after standing for long periods of time, but improves with elevation or by using compression stockings.
Arterial 1,2
When the arteries are not able to pump blood efficiently, it can lead to pooling of blood in the legs and painful side effects.1 This pain and aching in the leg muscles may occur when walking or climbing stairs, making it feel as if you are walking with heavy weights on your legs. The throbbing can radiate throughout the leg, but generally stops when exercise or motion ceases.2 These symptoms can range depending on the underlying PVD disease and how far it has progressed. If you are experiencing any of these symptoms consistently, it is important to take the step and seek help from your doctor. Early diagnosis and treatment can help to alleviate some of the discomfort and may help restore quality of life.
Causes
PVD diseases of the veins and arteries can lead to tired, heavy legs, but in different ways.
Superficial veins have less muscle support than deep veins, so any condition that puts pressure on the legs or surrounding areas can lead to pooling of blood.
Venous Causes
Over time, legs can begin to feel tired because of the increased venous pressure when blood is not being returned efficiently to the heart.3 Standing for long periods of time may exacerbate the symptoms, making it difficult to move and go about normal activities by the end of the day.
Arterial Causes
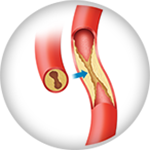
When PVD is the result of arterial conditions, it is caused by fatty plaque build-up in the arteries. The plaque can harden and reduce the flow of blood to the limbs.1 As people walk, their leg muscles need more oxygen, which the body must work harder to deliver. This leads to the aching, heavy feeling experienced by many with PAD.
Risk Factors

Tired, heavy legs can affect just about anyone. But some individuals have a higher risk of developing the symptom. These risk factors include:1,4
What to Look For
Sometimes it can be difficult to tell one symptom from another. If you think you may have tired, heavy, legs it is important to take the step to consult a doctor to help you obtain acorrect diagnosis. Signs of heaviness in legs include:
Associated Symptoms
Varicose Veins
Varicose veins can become inflamed when the pooling of blood results in pressure on the vein walls resulting in redness, swelling, and a diffuse pain.
Claudication
Pain, achiness or swelling occurs in the leg muscles when exercising or walking, but subsides at rest.
Swelling
Without adequate blood flow, extra fluid can begin to collect in the tissue, causing puffiness and swelling in one leg or both.
When to See a Doctor
Heaviness in the legs can signal PVD, which only progresses with time. If you are experiencing these symptoms, you should take the next step by talking to your doctor. If you do not have a doctor, you can use our tool to locate one nearby to get the help you need.
Helpful Resources

PVD Doctor
Discussion Guide
Get helpful tips and advice on how to talk to your doctor about a PVD screening.

Patient Brochures
Third-Party Resources
Helpful Websites
Blogs
Apps
A mobile app built by cardiologists, to simplify understanding of most cardiac and peripheral vascular conditions and treatments.
Find a Doctor
If you think you are experiencing exercise pain, it is important to get help. Talk to your doctor, or use our tool below to find a specialist near you.
Are You a Healthcare Professional?
Find out how to register your practice with us.
1. “Peripheral Artery Disease.” National Heart, Lung and Blood Institute. U.S. Department of Health and Human Services. June 22, 2016. 2. “Claudication.” Mayo Clinic. Jan. 31, 2015. Henke, P. 3. “Chronic Venous Insufficiency.” Society for Vascular Surgery. n.d. 4. “Venous insufficiency.” MedlinePLUS. U.S. National Library of Medicine. June 6, 2016. 5. “Chronic Venous Insufficiency.” John Hopkins Medicine. n.d.
Disclaimer
The opinions and clinical experiences presented herein are for informational purposes only. Individual results may vary depending on a variety of patient-specific attributes and related factors. Dr. Raghu Kolluri has been compensated by Philips for his services in preparing and providing this material for Philips further use and distribution. We offer links to third-party websites that may be of interest to our website visitors and in no way, represent any affiliation or endorsement of the information provided on those linked websites. These links are provided solely for your convenience and to assist you in learning more information on this topic. However, Philips does not control, endorse or guarantee the accuracy of the information contained on the linked sites. In addition, Philips makes no representations or warranties of any kind with regards to any third-party websites or information contained therein. If you have any questions or concerns about the information on the linked third-party websites, please contact the third-party websites directly.