Spider, Reticular & Varicose Veins
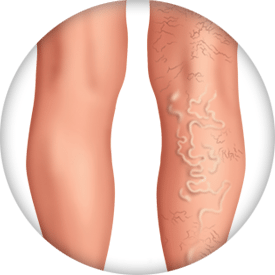
When veins become abnormally thick, full of twists and turns, or enlarged, they are called varicose veins. Spider veins are smaller feather-like veins on the surface that have been effected, while reticular, or “feeder veins” are smaller branches that lead to larger veins. These venous conditions are often symptoms of superficial venous insufficiency (SVI). Varicose veins may appear on the thighs, backs of the calves, or the inside of the legs. Although not life-threatening, varicose veins can progress to skin changes, wounds and other more serious conditions.1,2
Spider Veins
Spider veins, also known as telangiectasias, are small veins (less than 1mm) that can be seen on the surface of the skin and resemble tree branches with short, jagged lines. They are considered a milder form of varicose veins and differ in appearance, ranging from pink, red to bluish purple. Approximately 10 to 25 percent of the general adult population has spider veins, which is the result of stretched veins closer to the surface of the skin.6 As veins stretch from surrounding pressure, they can hold more blood and can become visible in common areas such as the calves, legs and face. Some individuals may not experience symptoms, while others may feel pain, throbbing or general discomfort in the affected area.
Reticular Veins
Reticular veins are small, blue or green dilated veins that appear 1 mm to 3 mm in diameter in areas such as the legs and the face.6 These common veins are typically smaller than varicose veins but larger than spider veins and appear flatter and less twisted. When such reticular veins are associated with spider veins, they are called “feeder veins.” Like spider veins and varicose veins, reticular veins are caused by weak or damaged valves in the veins. Blood can pool in the affected area and cause the dilated veins to appear beneath the skin. Reticular veins are often accompanied by significant symptoms of local tenderness or burning and itching.
Varicose Veins
Varicose veins are dilated veins larger than 3 mm in diameter that appear beneath the skin. The veins can be purple and blue and can occur in various areas throughout the body: thighs, legs, ankles, and feet. Varicose veins can bulge out above the surface of the skin. Similar to spider and reticular veins, varicose veins are a result of pooled blood that has become stagnant due to inefficient blood flow. The pooled blood creates pressure and surrounding inflammation in the vein, which can lead to aching, pain, burning and cramping.
Causes
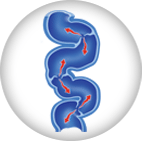
Normal, healthy veins have one-way valves that keep blood moving toward the heart. But when the valves in the superficial veins of the legs and feet are not working properly, the blood can pool into the lower extremities.3,4 The pooling of blood creates surrounding pressure and swelling internally, which may result in enlarged blue, red or flesh-colored vein that can be seen through the skin. Over time, this can lead to other changes to the texture of the skin, and ultimately leg ulcers, if not treated properly. Prolonged standing, pregnancy, obesity, straining, trauma, heredity or age can contribute to the development and progression of varicosities. Learn more about varicose vein risk factors.
Varicose Vein Risk Factors

There are many risk factors that may predispose a person to developing spider, reticular, or varicose veins. These risk factors include: 5,7
What to Look For
Venous disease is a progressive condition that may start out with mild to no signs. With time, it may lead to moderate or even severe symptoms such as heaviness, aching, swelling, tiredness, and itching, which can lead to a leg ulceration. The CEAP Classification is a common system that is widely used to diagnose and identify the severity of varicose veins as they progress with time.6
Rutherford Classification10
| | | | | | |
 |  |  |  |  |  |
Associated Symptoms
Edema in the Ankle
When blood flow is interrupted, the surrounding pressure on the veins can lead to edema, or swelling in the extremities, especially the ankles. This is the result of fluid build-up in one or both legs. The surrounding pressure can lead to uncomfortable symptoms such as heaviness, tightness, and overall discomfort. These symptoms may be relieved by elevating the legs or using compression stockings.
Skin Changes
As venous disease progresses, increased swelling and pressure occurs, and the skin around the legs can begin to deteriorate. The skin can become pigmented, dry, and thick (lipodermatosclerosis) and easily break down. The inflammation can lead to pain and significant discomfort the more severe the venous insufficiency.
Venous Ulcers
Without treatment of venous disease, increased swelling and skin inflammation due to poor circulation of blood flow can lead to serious complications8. The skin can break down and result in an open wound that requires medical attention. When the sores are open, they allow for bacteria and air to enter the wound, which can make the condition worse. Most venous ulcers occur above the ankle and can be slow to heal. They are often accompanied with leg pain, skin discoloration, and sores that seep pus and a bad odor if infection has set in.
When to See a Doctor
If self-care techniques such as exercise, lifting your legs while sitting and/or wearing compression stockings have not worked and/or you wish for cosmetic improvement of your veins, make an appointment to see your doctor to discuss next steps. It is important to seek help right away if you have developed a leg ulcer or other non-healing wounds because of SVI.
Associated PVD Diseases
Helpful Resources

PVD Doctor
Discussion Guide
Get helpful tips and advice on how to talk to your doctor about a PVD screening.

Third-Party Resources
Helpful Websites
Blogs
Find a Doctor
Consult your doctor to learn more about varicose veins and SVI and how to maintain your vein health. You can also use our tool below to find an SVI specialist near you.
This tool is not inclusive of all specialists. Consult with your insurance provider to find specialists that are covered within your network.
Are You a Healthcare Professional?
Find out how to register your practice with us.
1. Weiss et al. “Venous Insufficiency.” Medscape. May 26, 2016 2. Eberhardt et al. “Chronic Venous Insufficiency.” Circulation. 2014;130:333-346. July 21, 2014. 3. “Varicose veins and spider veins.” Office on Women’s Health. U.S. Department of Health and Human Services. January 04, 2017. 4. Lin et al. “The Management of Varicose Veins.” Int Surg. 2015 Jan; 100(1): 185–189. 5. “Who is at Risk for Varicose Veins?” National Heart, Lung and Blood Institute. U.S. Department of Health & Human Services. Jan. 29, 2016. 6. “What is CEAP?” American College of Phlebotomy. 7. “Minimally invasive treatments for bothersome leg veins,” Harvard Women’s Health Watch. Harvard Medical School Publications. April 2011. 8. “Venous ulcers.” Medline Plus. U.S. National Library of Medicine. May 24, 2016.
Disclaimer
The opinions and clinical experiences presented herein are for informational purposes only. Individual results may vary depending on a variety of patient-specific attributes and related factors. Dr. Raghu Kolluri has been compensated by Philips for his services in preparing and providing this material for Philips further use and distribution. We offer links to third-party websites that may be of interest to our website visitors and in no way, represent any affiliation or endorsement of the information provided on those linked websites. These links are provided solely for your convenience and to assist you in learning more information on this topic. However, Philips does not control, endorse or guarantee the accuracy of the information contained on the linked sites. In addition, Philips makes no representations or warranties of any kind with regards to any third-party websites or information contained therein. If you have any questions or concerns about the information on the linked third-party websites, please contact the third-party websites directly.





